mann assessment of swallowing ability pdf
Article Plan: Mann Assessment of Swallowing Ability (MASA) PDF
This article details the MASA, a bedside dysphagia assessment, exploring its history, administration, scoring, and comparison to other evaluations like FEES and CSE.
It also covers the modified MASA (mMASA), reliability studies, clinical applications in stroke and neurological disorders, and access to PDF resources.
Dysphagia, the medical term for swallowing difficulties, significantly impacts patient safety and quality of life. It can lead to aspiration pneumonia, malnutrition, and dehydration, increasing morbidity and mortality rates. Early and accurate assessment is crucial, particularly post-stroke or with neurological conditions like Parkinson’s and Multiple Sclerosis.
Nurses play a vital role in initial dysphagia screening, as highlighted by the Joint Commission’s focus on early identification. A comprehensive assessment, such as the Mann Assessment of Swallowing Ability (MASA), provides valuable clinical information to guide appropriate interventions, including dietary modifications and swallowing therapy.
What is the Mann Assessment of Swallowing Ability (MASA)?
The Mann Assessment of Swallowing Ability (MASA) is a standardized, bedside evaluation tool designed to identify individuals at risk for dysphagia. Developed by Maggie Mann in 1999, it’s a quick, practical method for clinicians to assess swallowing function using readily available materials – no specialized equipment is required.
MASA focuses on clinical observation throughout the oral, pharyngeal, and potentially, initial esophageal phases of swallowing. It’s a valuable screening tool, offering a total score that indicates the level of dysphagia risk, guiding further diagnostic evaluations if needed.
Historical Context of the MASA
The MASA emerged from a need for a simple, accessible dysphagia screening tool. Maggie Mann initially developed and published the assessment in 1999, recognizing a gap in readily available methods for initial swallowing evaluation.
Over time, the MASA has undergone revisions and adaptations, leading to the modified MASA (mMASA) to address specific patient populations, particularly those with cognitive impairment. Its continued use reflects its practicality and value in clinical settings, despite advancements in other dysphagia assessment techniques.
Development and Original Publication (1999)
Maggie Mann’s initial work focused on creating a practical bedside assessment for identifying individuals at risk of dysphagia. The 1999 publication of the MASA provided clinicians with a standardized, easily administered tool.
This original version prioritized clinical observation of swallowing function across different bolus consistencies. It aimed to quickly identify patients needing further, more detailed evaluation, like FEES. The MASA’s development stemmed from real-world clinical needs and a desire for efficient dysphagia screening.

Evolution and Updates to the Assessment
Following its initial release, the MASA underwent refinements based on clinical feedback and research findings. This led to the development of the modified MASA (mMASA), specifically addressing the challenges of assessing patients with cognitive impairment, such as those with dementia.
The mMASA incorporates adaptations to account for reduced attention spans and communication difficulties. Ongoing research continues to evaluate and potentially refine the MASA, ensuring its continued relevance and accuracy in dysphagia assessment.
Purpose and Goals of the MASA
The primary purpose of the MASA is to quickly identify individuals at risk of dysphagia, particularly following stroke or with neurological conditions. It aims to provide a standardized, bedside assessment to determine the need for further, more detailed evaluation, such as a FEES or a full clinical swallow evaluation.
The MASA’s goals include early detection of swallowing difficulties, minimizing aspiration risk, and guiding appropriate dietary recommendations and rehabilitation strategies. It supports safe and effective patient care;

Key Features of the MASA
A defining feature of the MASA is its bedside nature, requiring minimal equipment and allowing for rapid assessment at the point of care. It heavily relies on clinical observation of the patient’s swallowing function across different bolus consistencies – liquids, purees, and solids.
The MASA is designed for ease of use by trained healthcare professionals, offering a practical tool for initial dysphagia screening. It doesn’t require specialized instrumentation, making it accessible in various clinical settings.
Bedside Assessment Nature
The MASA’s core strength lies in being a bedside assessment, meaning it’s conducted at the patient’s bedside, avoiding the need for transport to radiology or specialized labs. This accessibility allows for quick initial evaluation, crucial in acute care settings like stroke units.
It minimizes disruption to the patient and streamlines the diagnostic process. The MASA doesn’t necessitate complex equipment, relying instead on the clinician’s observational skills and readily available food textures.
Focus on Clinical Observation
The MASA heavily emphasizes detailed clinical observation during all phases of the swallow. Clinicians meticulously assess the patient’s ability to handle food and liquid, noting any signs of aspiration risk – such as coughing, choking, or wet vocal quality.
This observational approach allows for a dynamic assessment, capturing subtle cues that might be missed by purely instrumental methods. The MASA prioritizes identifying immediate safety concerns and guiding initial dietary recommendations.
Components of the MASA
The MASA systematically evaluates three key phases of swallowing: oral preparatory, oral, and pharyngeal. The oral preparatory phase assesses lip closure, cheek tension, and bolus formation. The oral phase examines bolus propulsion and transit time;
Finally, the pharyngeal phase focuses on triggering the swallow reflex, laryngeal elevation, and airway protection. Each phase is carefully observed with varying bolus consistencies – liquids, purees, and solids – to identify potential impairments.
Oral Preparatory Phase Assessment
This initial MASA component focuses on preparing food for swallowing; Clinicians observe lip closure – ensuring a seal to prevent leakage – and cheek tension to maintain bolus integrity. Bolus formation, the ability to manipulate food into a cohesive mass, is also assessed.
Observations include the patient’s ability to handle different textures and the time taken to form a bolus. Deficits here can indicate difficulties initiating the swallow and potential aspiration risk.
Oral Phase Assessment

The MASA’s oral phase assessment examines bolus transport. Clinicians observe the tongue’s movement, ensuring it efficiently moves the bolus posteriorly. Residue within the oral cavity after the swallow is noted, indicating incomplete clearance.
Assessment includes observing for pocketing (food accumulating in cheeks) and premature spillage. Difficulty initiating or coordinating the tongue movement suggests potential aspiration. This phase is crucial for a safe and effective swallow.
Pharyngeal Phase Assessment
The MASA’s pharyngeal assessment focuses on swallow initiation and airway protection. Clinicians observe for laryngeal elevation and the presence of a cough before the swallow, indicating potential silent aspiration. Hyolaryngeal excursion, the upward movement of the larynx, is also evaluated.
Signs of concern include delayed swallow initiation, weak pharyngeal contraction, and residue in the pharynx post-swallow. Assessing these elements helps determine the risk of aspiration during this critical phase of swallowing.
Scoring System of the MASA
The MASA utilizes a simple scoring system based on observed clinical signs during each swallowing phase. Each phase – oral preparatory, oral, and pharyngeal – receives a score reflecting the patient’s performance. A total score is calculated, providing an overall indication of swallowing ability.
Higher scores suggest greater impairment, while lower scores indicate more efficient swallowing. Clinicians use these scores to categorize dysphagia risk and guide appropriate interventions, such as dietary modifications or further diagnostic testing.
Total Score Interpretation
The MASA’s total score provides a crucial snapshot of a patient’s swallowing function. Scores range, indicating varying degrees of dysphagia severity. A low score generally suggests intact swallowing mechanisms, while progressively higher scores correlate with increasing risk of aspiration and penetration.
Clinicians interpret the total score in conjunction with observed clinical signs to determine appropriate management strategies. This includes dietary texture modifications, swallowing exercises, and recommendations for further evaluation, like a FEES study.
Cut-off Scores for Dysphagia Risk
Establishing clear cut-off scores is vital for identifying patients at risk of dysphagia. While specific thresholds can vary based on clinical context, a score of 8 or higher on the MASA often indicates a significant risk of aspiration.
Scores between 4 and 7 suggest a moderate risk, warranting close monitoring and potential dietary adjustments. Lower scores (below 4) typically indicate minimal dysphagia risk, though ongoing assessment remains important, especially post-stroke.
Administration of the MASA
Administering the MASA requires a quiet environment and a trained clinician. The assessment is performed at the bedside, observing the patient through the three phases of swallowing – oral preparatory, oral, and pharyngeal.
Standardized food textures and liquid viscosities are utilized, progressing as tolerated. Careful observation of signs like coughing, choking, or wet vocal quality is crucial. Documentation of observations is essential for accurate scoring and treatment planning.
Required Materials and Equipment
For MASA administration, several materials are essential. These include a standardized case history form for patient details, and a variety of food textures – pureed, mechanically altered, and regular – alongside different liquid viscosities (thin, honey-thick, pudding-thick).
A stopwatch is needed for timing observations, and a penlight to assess oral motor function. A cup, spoon, and napkins are also required, alongside a method for documenting observations accurately during the assessment process.
Step-by-Step Procedure Guide
Begin with a case history review, then assess the patient’s alertness and orientation. Start with oral preparatory and oral phases, observing lip closure, tongue movement, and bolus formation with each texture.

Progress through liquid viscosities, noting any signs of aspiration or residue. Evaluate the pharyngeal phase by observing swallow initiation and airway protection. Document all observations meticulously, scoring each phase based on the MASA criteria for a comprehensive assessment.
MASA vs. Other Dysphagia Assessments
The MASA is a quick, bedside clinical swallow evaluation (CSE), differing from the more invasive Fiberoptic Endoscopic Evaluation of Swallowing (FEES). While FEES directly visualizes the pharynx, the MASA relies on clinical observation of swallowing function.
MASA offers a broader, initial screening, while FEES provides detailed anatomical information. MASA’s simplicity makes it accessible, but it may lack the sensitivity of FEES in detecting subtle aspiration risks, necessitating further investigation when indicated.
Comparison with Clinical Swallow Evaluation (CSE)
Both the MASA and CSE are bedside assessments, relying on clinical observation during swallowing. However, the MASA provides a standardized scoring system, offering a more objective measure compared to the typically descriptive CSE report.
CSE is often more flexible, allowing for a tailored evaluation, while MASA’s structured approach enhances consistency. Nurses frequently utilize CSE for initial screening, and the MASA can supplement this with quantifiable data, aiding in dysphagia risk stratification.
Comparison with Fiberoptic Endoscopic Evaluation of Swallowing (FEES)

FEES is an instrumental assessment, providing a direct visualization of the pharyngeal phase, unlike the MASA’s observational nature. FEES identifies residue and laryngeal anatomy with greater detail, but requires specialized training and equipment.
MASA serves as a valuable initial screening tool, helping determine the need for a more in-depth FEES evaluation. While MASA assesses overall risk, FEES pinpoints specific impairments. Combining both offers a comprehensive dysphagia profile for optimal patient care.
Modified Mann Assessment of Swallowing Ability (mMASA)
The mMASA addresses limitations of the original MASA in patients with cognitive impairment, particularly dementia. Adaptations simplify instructions and reduce reliance on complex commands, enhancing patient participation.
This modified version maintains core assessment components, but allows for caregiver assistance and accepts responses beyond verbalization. Studies explore the correlation between MASA and mMASA scores across varying cognitive levels, aiming to improve diagnostic accuracy in vulnerable populations.
Addressing Cognitive Impairment

Cognitive deficits significantly impact swallowing assessment accuracy. The mMASA directly tackles this by simplifying task instructions and reducing the cognitive load on patients. It allows for cues and assistance from caregivers, acknowledging the patient’s limitations.
The assessment accepts non-verbal responses, recognizing that patients with dementia may struggle with clear communication. This adaptation enhances participation and provides a more realistic evaluation of their swallowing function, improving diagnostic reliability.
Adaptations for Patients with Dementia
Patients with dementia often exhibit fluctuating attention and memory, necessitating specific mMASA adjustments. The assessment prioritizes a calm, familiar environment to minimize agitation and maximize cooperation. Simplified instructions and repetition are key, alongside allowing ample time for response.
Caregiver input is crucial, providing insights into the patient’s usual swallowing patterns and cognitive abilities. The mMASA focuses on observable behaviors, reducing reliance on patient self-report, ensuring a more accurate and sensitive evaluation.
Reliability and Validity of the MASA
Establishing the MASA’s trustworthiness is paramount. Inter-rater reliability studies demonstrate acceptable agreement among clinicians administering the assessment, ensuring consistent scoring. Sensitivity and specificity data indicate the MASA’s ability to correctly identify individuals with and without dysphagia.
However, it’s crucial to acknowledge limitations; the MASA is a screening tool, not a definitive diagnostic test. Further instrumental assessments, like FEES, may be needed for comprehensive evaluation and to confirm findings.
Inter-Rater Reliability Studies
Numerous studies have investigated the consistency of MASA scoring between different clinicians. These investigations typically involve multiple raters independently assessing the same patients using the MASA protocol. Statistical analysis, such as Kappa coefficients, is then employed to quantify the level of agreement.
Results generally show acceptable to good inter-rater reliability, suggesting the MASA provides relatively consistent results regardless of who administers it. However, proper training and adherence to standardized procedures are vital for maximizing reliability.
Sensitivity and Specificity Data
Evaluating the MASA’s diagnostic accuracy requires examining its sensitivity and specificity. Sensitivity reflects the assessment’s ability to correctly identify individuals with dysphagia, while specificity indicates its ability to correctly identify those without the condition.
Published data suggests moderate sensitivity and specificity, meaning the MASA isn’t perfect at detecting all cases or ruling them out. It’s best used as an initial screening tool, with positive results prompting further, more definitive evaluation like FEES.
Clinical Applications of the MASA
The MASA finds broad application in various clinical settings, particularly in stroke rehabilitation where dysphagia is prevalent. It’s valuable for quickly identifying patients at risk, guiding initial dietary modifications, and determining the need for instrumental assessments.
Furthermore, the MASA is utilized in managing neurological disorders like Parkinson’s disease and Multiple Sclerosis, where swallowing impairment commonly occurs. Its ease of administration makes it suitable for routine screening in these populations, improving patient safety and care.
Stroke Rehabilitation
Following a stroke, dysphagia is a frequent complication, impacting nutrition and increasing pneumonia risk. The MASA serves as a crucial initial screening tool within stroke rehabilitation programs, enabling rapid identification of swallowing deficits.
Nurses, central to stroke care, utilize the MASA for early detection, informing decisions about diet texture and fluid consistency. This proactive approach minimizes aspiration risk and supports optimal recovery. The MASA guides referrals for more detailed evaluations, like FEES, when necessary.
Neurological Disorders (Parkinson’s, MS)
Dysphagia frequently accompanies progressive neurological conditions like Parkinson’s Disease and Multiple Sclerosis (MS). The MASA provides a practical assessment for identifying swallowing impairments in these populations, where subtle deficits can significantly impact quality of life.
Regular MASA administration helps monitor disease progression and adjust dietary recommendations accordingly. It aids in preventing aspiration pneumonia, a serious concern for individuals with weakened swallowing muscles. The assessment’s simplicity makes it suitable for ongoing evaluation in neurological settings.
Limitations of the MASA
While valuable, the MASA is a bedside assessment and lacks the detailed visualization offered by instrumental evaluations like FEES. It relies heavily on clinical observation, potentially missing subtle aspiration risks. MASA’s sensitivity can be affected by patient alertness and cooperation, particularly in cognitive impairment.
The assessment doesn’t evaluate all aspects of the swallow, such as laryngeal elevation or hyoid bone movement. Therefore, a normal MASA score doesn’t definitively rule out dysphagia; further investigation may be necessary for complex cases.
Accessing the MASA PDF and Resources
Currently, a freely available, official MASA PDF form is difficult to locate directly online. Resources often point to purchasing the assessment through specific vendors or professional organizations. However, various institutions may have internal copies for clinical use.
Training opportunities for MASA administration are typically offered through continuing education courses focused on dysphagia management. Exploring professional speech-language pathology associations can reveal relevant workshops and certification options for enhanced competency.
Online Availability of the Assessment Form
Locating a readily downloadable MASA PDF form presents a challenge. While numerous websites discuss the assessment, a direct link to a free, official version is scarce. Many resources direct users to purchase the form through specialized medical supply companies or professional organizations focused on speech pathology.
Unofficial versions may exist, but their validity and accuracy are questionable. Clinicians should prioritize obtaining the assessment from reputable sources to ensure proper administration and reliable results.
Training and Certification Opportunities
Formal certification for MASA administration isn’t universally mandated, however, comprehensive training is highly recommended. Workshops and continuing education courses, often offered by speech-language pathology organizations, provide in-depth instruction on proper technique and interpretation.
These programs ensure clinicians understand the nuances of bedside swallowing assessments and can accurately utilize the MASA scoring system. Seeking training enhances clinical competence and patient safety when identifying dysphagia risk.
MASA and Nursing Practice in Dysphagia Care
Nurses play a crucial role in early dysphagia detection, and the MASA empowers them to initiate timely screening, particularly post-stroke. While not a replacement for SLP evaluation, the MASA provides valuable preliminary data.

This allows for swift referral and intervention, minimizing aspiration risk. Consistent MASA implementation, coupled with ongoing education, improves nursing’s contribution to comprehensive dysphagia management and patient outcomes.
Correlation Studies: MASA and Modified MASA (mMASA)
Research investigates the relationship between the standard MASA and its modified version (mMASA), particularly concerning cognitive impact on assessment results. Studies aim to determine if the mMASA accurately reflects swallowing ability in patients with cognitive impairment, like dementia.
Findings explore whether scores differ significantly based on cognitive status, informing clinical decisions and optimizing assessment selection for diverse patient populations. These correlations help refine the MASA’s application.
MANN-FILTER and its Relevance (Indirect Connection ― Filter Technology & Health)
While seemingly unrelated to dysphagia assessment, MANN-FILTER’s expertise in filtration highlights the broader importance of filtering in health. Their advanced filtration technology protects engines, mirroring the body’s natural defense mechanisms against harmful substances.
This connection underscores the significance of preventing aspiration – a key focus of the MASA – as it’s essentially a ‘filtration failure’ within the swallowing process. MANN-FILTER’s commitment to purity and protection subtly parallels healthcare’s goal of maintaining physiological wellbeing.
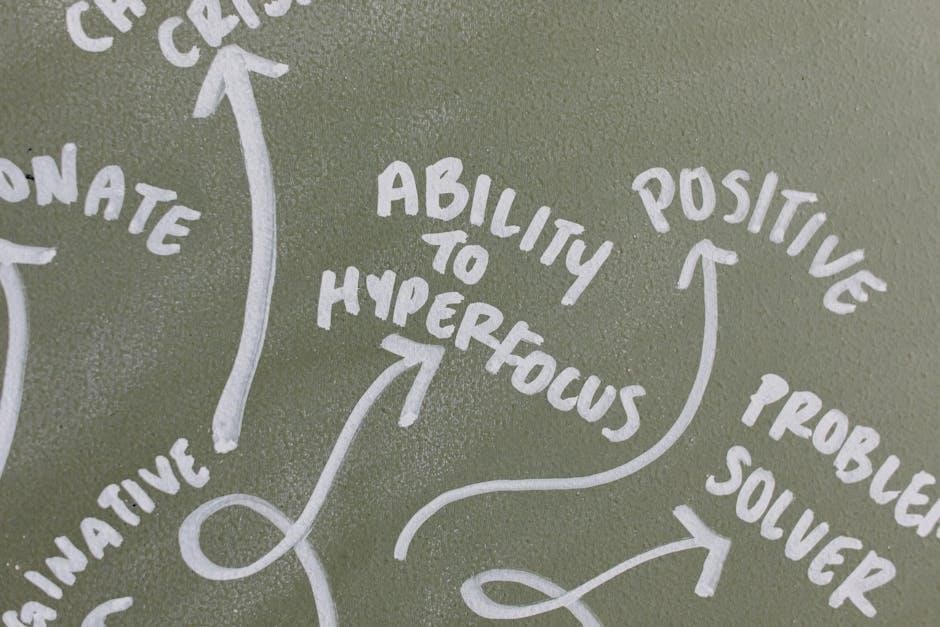
Dhar Mann’s Work and Positive Impact (Indirect Connection ⸺ Health & Wellbeing)
Dhar Mann’s focus on inspiring and uplifting stories indirectly connects to the holistic care surrounding dysphagia. His content promotes wellbeing and positive change, mirroring the rehabilitation goals for patients undergoing swallowing therapy post-assessment with tools like the MASA;
Improved quality of life is central to both Mann’s message and dysphagia management. Addressing swallowing difficulties enhances nutrition, social interaction, and overall health, aligning with Mann’s emphasis on a positive outlook and personal growth.
MANNHUMMEL’s Role in Filtration Technology (Indirect Connection ⸺ Health & Wellbeing)
MANNHUMMEL, a global filtration expert, indirectly relates to health through its development of innovative solutions. While seemingly distant from swallowing assessments like the MASA, filtration technology is crucial in maintaining sterile environments within healthcare settings.
Clean air and water are fundamental to patient recovery, including those with dysphagia. MANNHUMMEL’s products contribute to a safer healthcare ecosystem, supporting optimal conditions for diagnosis, treatment, and rehabilitation – indirectly bolstering the effectiveness of assessments like the MASA.
Mann Oil Filters and Engine Health (Indirect Connection ― Health & Wellbeing)
Although seemingly unrelated to the Mann Assessment of Swallowing Ability (MASA), maintaining vehicle health via Mann oil filters contributes to reliable transportation for healthcare access. Consistent access to medical facilities is vital for individuals requiring dysphagia evaluations and ongoing care.
Reliable transportation ensures patients can attend appointments, receive therapies, and manage their condition effectively. MANN-FILTER’s commitment to engine protection indirectly supports patient wellbeing by facilitating access to essential healthcare services, including those related to swallowing difficulties.
Future Directions in Dysphagia Assessment and the MASA
Ongoing research focuses on refining the MASA’s sensitivity and specificity, particularly in diverse patient populations. Exploring integration with telehealth platforms could expand access to initial dysphagia screening, especially in remote areas. Further investigation into the correlation between MASA and modified MASA (mMASA) scores, considering varying cognitive levels, is crucial.
Development of standardized training programs for MASA administration will enhance inter-rater reliability. Ultimately, advancements aim to create a more efficient and accurate initial assessment tool, improving patient outcomes and care pathways.
